
Because I took 2 DNA test (23andMe and Ancestry®) I decided to get a complete DNA break down of my health. In doing so I found a ton of data which gave me a greater understanding of my health as well as the history of human adaptation and health.
So, in this time of COVID-19 how relevant is DNA research? The followings is what 23andMe under 23andMe Research has to offer.
Coronavirus is a general term that includes many different (but related) viruses, including the one causing the current pandemic.
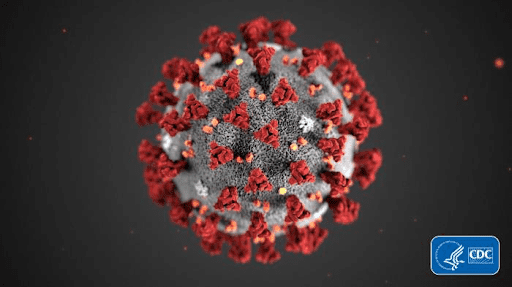
COVID-19 is the disease caused by the novel coronavirus. COVID-19 stands for coronavirus disease 2019 (the year the virus was first found in humans).
What are viruses? What's the difference between a bacterium and a virus?
The world around us is full of viruses and bacteria, which are often harmless. But not always — both of these types of germs can also infect people and make us sick. Although each bacterium (the singular form of "bacteria") is only a single cell, bacteria are living organisms that can survive and reproduce on their own in all kinds of conditions, even without a host. Viruses, on the other hand, aren't truly alive at all — they're just a small piece of DNA or RNA wrapped in a protein shell, sometimes wrapped in another fatty coating. The only way they reproduce is by entering a host's cells and hijacking cellular machinery to create more viruses. In fact, there are even viruses that infect bacteria.
Could genetics play a role in the severity of COVID-19?
April 8, 2020 By 23andMe under 23andMe Research
Scientists around the world are racing to understand COVID-19 and the novel coronavirus that causes the disease. Among the questions they’re asking: Why do most people who are infected show mild to moderate symptoms (or possibly no symptoms at all), whereas others develop severe disease?
We know that certain factors — like advanced age or underlying health conditions like heart disease and diabetes — can make someone more likely to develop severe symptoms, including pneumonia. But even young, healthy people can develop severe symptoms and die from COVID-19. Why might that be?
Could genetics play a role?
With the help of our research participants, 23andMe is launching a research study to try to answer that question. Before we describe 23andMe’s planned research, here’s some of what is known about the role of genetics in other infectious diseases.
Human genetics plays a role in many infectious diseases
We know from past research that genetics can influence a person’s susceptibility to different infectious diseases — including whether they’re infected and how severe their disease becomes.
For example:
- Particular genetic variants in a gene called HBB can make people less susceptible to infection by the parasite that causes malaria. HBB contains instructions for making the hemoglobin protein that carries oxygen inside our red blood cells.
- A particular genetic variant in a gene called CCR5 can protect people from HIV infection by preventing the virus from being able to enter certain T cells in our immune system. CCR5 codes for a protein that sits on the surface of those T cells.
- People with a particular variant in the FUT2 gene are much less likely to be infected by norovirus. FUT2 codes for an enzyme that helps determine whether certain molecules are present on the surface of our gut cells.
In addition, genetic variants in HLA genes may explain the differences in response to several different conditions. This group of genes helps the immune system distinguish the body’s own proteins from proteins made by foreign invaders like viruses and bacteria. Studies have found that variants in these genes may help explain why HIV progresses more quickly in some people than others. Variants in the HLA genes may also influence why some people can clear hepatitis B infection and others don’t, instead ending up with a chronic disease. And variants in this same group of genes could offer insight into why some (but not all) people infected with dengue virus experience severe complications. In 2017, scientists at 23andMe published a genetic study that identified almost 60 genetic variants associated with susceptibility to one of 17 different infectious diseases, and many of those variants were in HLA genes.
What about COVID-19?
So, could genetics help explain why certain people develop severe COVID-19 and others develop only mild or undetectable symptoms?
It’s too early to say for sure, but some scientists think that’s likely the case. At least a couple of studies have started looking for clues.
For example, in order to get inside our cells, the virus that causes COVID-19 latches onto a human protein called ACE2. And scientists identified genetic variants in and near the ACE2 gene that could impact how much ACE2 protein is made, or how the protein functions. This could make it easier or tougher for the virus to slip inside a person’s cells and make them sick. In another study, scientists reported that a person’s blood type — which is determined by the ABO gene — might influence their likelihood of being infected by the virus. While these preliminary observations are intriguing, more research in different populations and in larger groups of patients is needed to validate these and other findings.
How 23andMe Research could make a difference
23andMe’s unique research model, with millions of customers consented to participate, offers our scientists a powerful tool for potential insight into the role genetics may play in explaining differences in the severity of the novel coronavirus.
One way to identify genetic variants that contribute to disease severity is a genome-wide association study or GWAS. In a GWAS, scientists compare the DNA of people who had severe symptoms to the DNA of people who had milder symptoms, or even no symptoms at all. Genetic variants that are more common in one of these groups of participants than the other represent genetic associations with COVID-19 severity.
And that’s just one question that 23andMe Research hopes to answer. We’ll compare genetic variants in people who get very sick with variants in people who had milder symptoms or haven’t gotten sick. By identifying genetic variants that are more common in people who experienced severe disease, scientists may be able to better understand who’s most at risk. Perhaps even more importantly, these genetic studies can also help us gain new insights into how the novel coronavirus infects our cells and impacts our bodies. And those insights might give us clues to potential targets for new drugs or vaccines.
Learn more about 23andMe’s study here.
No comments:
Post a Comment